Guía de Práctica Clínica
Hipertensión Arterial Primaria o Esencial en personas de 15 años y más.
T1- Recomendación / Juicio del Panel y Evidencia
T1.- En pacientes mayores de 70 años con hipertensión arterial, el Ministerio de Salud SUGIERE límite inferior de presión arterial diastólica en 70 mm de Hg por sobre límite inferior de presión arterial diastólica en 60 mm de Hg.
A continuación se presenta la “Tabla de la evidencia a la decisión” con el resumen de los juicios, la evidencia de investigación evaluada, consideraciones adicionales y comentarios planteados por el panel.
| No | Probablemente no | Probablemente sí | Sí | Varía | No lo sé |
|---|
El problema ha sido definido como prioritario en el marco de las Garantías Explícitas en Salud (GES), régimen integral de salud que prioriza un grupo de patologías o problemas de salud, garantizando el acceso a tratamiento oportuno y de calidad.
| Trivial | Pequeño | Moderado | Grande | Varía | No lo sé |
|---|
Moderados: El equipo elaborador de la Guía estimó que los efectos deseables de «Límite inferior de presión arterial diastólica (PAD) en 70 mm de Hg.» en comparación a «Límite inferior de presión arterial diastólica (PAD) en 60 mm de Hg.» son moderados, considerando la evidencia, experiencia clínica, conocimiento de gestión o experiencia de las personas con la condición o problema de salud.
El panel considera que es preferible un límite inferior PAD de 70 mm de Hg, según curva J (1), ya que podría disminuir la morbimortalidad en estos pacientes.
Evidencia de investigación
|
Límite inferior de presión arterial diastólica en 70 mm de Hg comparado con límite inferior de presión arterial diastólica en 60 mm de Hg |
|
|||
|
Población |
Personas mayores de 70 años con diagnóstico de hipertensión arterial |
|
||
|
Intervención |
Límite inferior de presión arterial diastólica en 70 mm de Hg |
|
||
|
Comparación |
Límite inferior de presión arterial diastólica en 60 mm de Hg |
|
||
|
Desenlaces |
Efecto |
Certeza de la evidencia (GRADE) |
Mensajes clave en términos sencillos |
|
|
Beneficio |
No se identificaron estudios que comparen el límite inferior de presión arterial en los rangos solicitados. |
— |
— |
|
|
Efectos adversos |
No se identificaron estudios que comparen el límite inferior de presión arterial en los rangos solicitados. |
–– |
— |
|
GRADE: Grados de evidencia Grading of Recommendations Assessment, Development and Evaluation.
Fecha de elaboración de la tabla: Julio, 2018
Referencia
2. Arguedas JA, Perez MI, Wright JM. Treatment blood pressure targets for hypertension. Cochrane Database of Systematic Reviews. 2009;(3):CD004349.
3. Bangalore S., Toklu B., Gianos E., Schwartzbard A., Weintraub H., Ogedegbe G., Messerli F.H.. Optimal Systolic Blood Pressure Target After SPRINT: Insights from a Network Meta-Analysis of Randomized Trials. American Journal of Medicine. 2017;130(6):707-719.e8.
4. Bangalore S, Kumar S, Lobach I, Messerli FH. Blood pressure targets in subjects with type 2 diabetes mellitus/impaired fasting glucose: observations from traditional and bayesian random-effects meta-analyses of randomized trials. Circulation. 2011;123(24):2799-810, 9 p following 810.
5. Bavishi C, Bangalore S, Messerli FH. Outcomes of Intensive Blood Pressure Lowering in Older Hypertensive Patients. Journal of the American College of Cardiology. 2017;69(5):486-493.
6. Brunström M, Carlberg B. Effect of antihypertensive treatment at different blood pressure levels in patients with diabetes mellitus: systematic review and meta-analyses. BMJ (Clinical research ed.). 2016;352:i717.
7. Czernichow S, Zanchetti A, Turnbull F, Barzi F, Ninomiya T, Kengne AP, Lambers Heerspink HJ, Perkovic V, Huxley R, Arima H, Patel A, Chalmers J, Woodward M, MacMahon S, Neal B, Blood Pressure Lowering Treatment Trialists’ Collaboration. The effects of blood pressure reduction and of different blood pressure-lowering regimens on major cardiovascular events according to baseline blood pressure: meta-analysis of randomized trials. Journal of hypertension. 2011;29(1):4-16.
8. Ettehad D, Emdin CA, Kiran A, Anderson SG, Callender T, Emberson J, Chalmers J, Rodgers A, Rahimi K. Blood pressure lowering for prevention of cardiovascular disease and death: a systematic review and meta-analysis. Lancet (London, England). 2016;387(10022):957-67.
9. Garrison SR, Kolber MR, Korownyk CS, McCracken RK, Heran BS, Allan GM. Blood pressure targets for hypertension in older adults. Cochrane Database of Systematic Reviews. 2017;8:CD011575.
10. Kaiser T, Florack C, Stephan U, Sawicki PT. Should BP targets be lower in diabetic patients with microalbuminuria or nephropathy? A systematic review of randomised controlled trials. British Journal of Diabetes & Vascular Disease. 2003;3(4):278-281.
11. Lee M, Saver JL, Hong KS, Hao Q, Ovbiagele B. Does achieving an intensive versus usual blood pressure level prevent stroke?. Annals of neurology. 2012;71(1):133-40.
12. Lv J, Ehteshami P, Sarnak MJ, Tighiouart H, Jun M, Ninomiya T, Foote C, Rodgers A, Zhang H, Wang H, Strippoli GF, Perkovic V. Effects of intensive blood pressure lowering on the progression of chronic kidney disease: a systematic review and meta-analysis. CMAJ: Canadian Medical Association journal = journal de l’Association medicale canadienne. 2013;185(11):949-57.
13. Lv J, Neal B, Ehteshami P, Ninomiya T, Woodward M, Rodgers A, Wang H, Macmahon S, Turnbull F, Hillis G, Chalmers J, Perkovic V. Effects of intensive blood pressure lowering on cardiovascular and renal outcomes: a systematic review and meta-analysis. PLoS medicine. 2012;9(8):e1001293.
14. Malhotra R, Nguyen HA, Benavente O, Mete M, Howard BV, Mant J, Odden MC, Peralta CA, Cheung AK, Nadkarni GN, Coleman RL, Holman RR, Zanchetti A, Peters R, Beckett N, Staessen JA, Ix JH. Association Between More Intensive vs Less Intensive Blood Pressure Lowering and Risk of Mortality in Chronic Kidney Disease Stages 3 to 5: A Systematic Review and Meta-analysis. JAMA internal medicine. 2017;177(10):1498-1505.
15. McBrien K, Rabi DM, Campbell N, Barnieh L, Clement F, Hemmelgarn BR, Tonelli M, Leiter LA, Klarenbach SW, Manns BJ. Intensive and Standard Blood Pressure Targets in Patients With Type 2 Diabetes Mellitus: Systematic Review and Meta-analysis. Archives of internal medicine. 2012;172(17):1296-303.
16. Moraes AAI, Baena CP, Muka T, Bano A, Buitrago-Lopez A, Zazula A, Erbano BO, Schio NA, Guedes MH, Bramer WM, Franco OH, Faria-Neto JR. Achieved systolic blood pressure in older people: a systematic review and meta-analysis. BMC geriatrics. 2017;17(1):279.
17. Saiz, Luis Carlos, Gorricho, Javier, Garjón, Javier, Celaya, Mª Concepción, Erviti, Juan, Leache, Leire. Blood pressure targets for the treatment of people with hypertension and cardiovascular disease. Cochrane Database of Systematic Reviews. 2018;7:CD010315.
18. Turnbull F, Blood Pressure Lowering Treatment Trialists’ Collaboration. Effects of different blood-pressure-lowering regimens on major cardiovascular events: results of prospectively-designed overviews of randomised trials. Lancet. 2003;362(9395):1527-35.
19. Upadhyay A, Earley A, Haynes SM, Uhlig K. Systematic review: blood pressure target in chronic kidney disease and proteinuria as an effect modifier. Annals of internal medicine. 2011;154(8):541-8.
20. Weiss J, Freeman M, Low A, Fu R, Kerfoot A, Paynter R, Motu’apuaka M, Kondo K, Kansagara D. Benefits and Harms of Intensive Blood Pressure Treatment in Adults Aged 60 Years or Older: A Systematic Review and Meta-analysis. Annals of internal medicine. 2017;166(6):419-429.
21. Weiss J, Kerfoot A, Freeman M, Motu’apuaka M, Fu R, Low A, Paynter R, Kondo K, Kansagara D. Benefits and Harms of Treating Blood Pressure in Older Adults: A Systematic Review and Meta-analysis. VA Evidence-based Synthesis Program Reports. 2016;
22. Xie X, Atkins E, Lv J, Bennett A, Neal B, Ninomiya T, Woodward M, MacMahon S, Turnbull F, Hillis GS, Chalmers J, Mant J, Salam A, Rahimi K, Perkovic V, Rodgers A. Effects of intensive blood pressure lowering on cardiovascular and renal outcomes: updated systematic review and meta-analysis. Lancet (London, England). 2016;387(10017):435-43.
23. Tsai WC, Wu HY, Peng YS, Yang JY, Chen HY, Chiu YL, Hsu SP, Ko MJ, Pai MF, Tu YK, Hung KY, Chien KL. Association of Intensive Blood Pressure Control and Kidney Disease Progression in Nondiabetic Patients With Chronic Kidney Disease: A Systematic Review and Meta-analysis. JAMA internal medicine. 2017;177(6):792-799
24. AASK (African American Study of Kidney Disease and Hypertension). Wright JT, Bakris G, Greene T, Agodoa LY, Appel LJ, Charleston J, Cheek D, Douglas-Baltimore JG, Gassman J, Glassock R, Hebert L, Jamerson K, Lewis J, Phillips RA, Toto RD, Middleton JP, Rostand SG. Effect of blood pressure lowering and antihypertensive drug class on progression of hypertensive kidney disease: results from the AASK trial. JAMA: the journal of the American Medical Association. 2002;288(19):2421-31.
25. ABCD-2V (Appropriate Blood Pressure Control in Diabetes Part 2 with Valsartan). Estacio RO, Coll JR, Tran ZV, Schrier RW. Effect of intensive blood pressure control with valsartan on urinary albumin excretion in normotensive patients with type 2 diabetes. American journal of hypertension. 2006;19(12):1241-8.
26. ABCD-H (Appropriate blood pressure control in diabetes (hypertensive)). Estacio RO, Jeffers BW, Gifford N, Schrier RW. Effect of blood pressure control on diabetic microvascular complications in patients with hypertension and type 2 diabetes. Diabetes care. 2000;23 Suppl 2:B54-64.
27. ABCD-N (Appropriate blood pressure control in diabetes (normotensive)). Schrier RW, Estacio RO, Esler A, Mehler P. Effects of aggressive blood pressure control in normotensive type 2 diabetic patients on albuminuria, retinopathy and strokes. Kidney international. 2002;61(3):1086-97.
28. ACCORD (Action to Control Cardiovascular Risk in Diabetes). Cushman WC, Evans GW, Byington RP, Goff DC, Grimm RH, Cutler JA, Simons-Morton DG, Basile JN, Corson MA, Probstfield JL, Katz L, Peterson KA, Friedewald WT, Buse JB, Bigger JT, Gerstein HC, Ismail-Beigi F. Effects of intensive blood-pressure control in type 2 diabetes mellitus. The New England journal of medicine. 2010;362(17):1575-85
29. BBB (Behandla Blodtryck Bättre [Treat Blood Pressure Better in Swedish]). Hannson L. The BBB Study: the effect of intensified antihypertensive treatment on the level of blood pressure, side-effects, morbidity and mortality in «well-treated» hypertensive patients. Behandla Blodtryck Bättre. Blood pressure. 1994;3(4):248-54.
30. Cardio-Sis (Italian Study on the Cardiovascular Effects of Systolic Blood Pressure Control). Verdecchia P, Staessen JA, Angeli F, de Simone G, Achilli A, Ganau A, Mureddu G, Pede S, Maggioni AP, Lucci D, Reboldi G, Cardio-Sis investigators. Usual versus tight control of systolic blood pressure in non-diabetic patients with hypertension (Cardio-Sis): an open-label randomised trial. Lancet. 2009;374(9689):525-33.
31. ESCAPE (Effect of Strict Blood Pressure Control and ACE Inhibition on the Progression of CRF in Pediatric Patients) ESCAPE Trial Group, Wühl E, Trivelli A, Picca S, Litwin M, Peco-Antic A, Zurowska A, Testa S, Jankauskiene A, Emre S, Caldas-Afonso A, Anarat A, Niaudet P, Mir S, Bakkaloglu A, Enke B, Montini G, Wingen AM, Sallay P, Jeck N, Berg U, Caliskan S, Wygoda S, Hohbach-Hohenfellner K, Dusek J, Urasinski T, Arbeiter K, Neuhaus T, Gellermann J, Drozdz D, Fischbach M, Möller K, Wigger M, Peruzzi L, Mehls O, Schaefer F. Strict blood-pressure control and progression of renal failure in children. The New England journal of medicine. 2009;361(17):1639-50.
32. HOMED-BP (Hypertension Objective treatment based on Measurement by Electrical Devices of Blood Pressure) Asayama K, Ohkubo T, Metoki H, Obara T, Inoue R, Kikuya M, Thijs L, Staessen JA, Imai Y, Hypertension Objective Treatment Based on Measurement by Electrical Devices of Blood Pressure (HOMED-BP). Cardiovascular outcomes in the first trial of antihypertensive therapy guided by self-measured home blood pressure. Hypertension research: official journal of the Japanese Society of Hypertension. 2012;35(11):1102-10.
33. HOT (Hypertension Optimal Treatment) Hansson L, Zanchetti A, Carruthers SG, Dahlöf B, Elmfeldt D, Julius S, Ménard J, Rahn KH, Wedel H, Westerling S. Effects of intensive blood-pressure lowering and low-dose aspirin in patients with hypertension: principal results of the Hypertension Optimal Treatment (HOT) randomised trial. HOT Study Group. Lancet. 1998;351(9118):1755-62.
34. INVEST (International Verapamil SR/Trandolapril Study) Pepine CJ, Handberg EM, Cooper-DeHoff RM, Marks RG, Kowey P, Messerli FH, Mancia G, Cangiano JL, Garcia-Barreto D, Keltai M, Erdine S, Bristol HA, Kolb HR, Bakris GL, Cohen JD, Parmley WW. A calcium antagonist vs a non-calcium antagonist hypertension treatment strategy for patients with coronary artery disease. The International Verapamil-Trandolapril Study (INVEST): a randomized controlled trial. JAMA: the journal of the American Medical Association. 2003;290(21):2805-16.
35. JATOS 2008 (JATOS 2008) JATOS Study Group. Principal results of the Japanese trial to assess optimal systolic blood pressure in elderly hypertensive patients (JATOS). Hypertension research: official journal of the Japanese Society of Hypertension. 2008;31(12):2115-27.
36. Lewis JB, Berl T, Bain RP, Rohde RD, Lewis EJ. Effect of intensive blood pressure control on the course of type 1 diabetic nephropathy. Collaborative Study Group. American journal of kidney diseases: the official journal of the National Kidney Foundation. 1999;34(5):809-17.
37. MDRD (Modification of Diet in Renal Disease) Sarnak MJ, Greene T, Wang X, Beck G, Kusek JW, Collins AJ, Levey AS. The effect of a lower target blood pressure on the progression of kidney disease: long-term follow-up of the modification of diet in renal disease study. Annals of internal medicine. 2005;142(5):342-51
38. Okin PM, Hille DA, Kjeldsen SE, Dahlöf B, Devereux RB. Impact of lower achieved blood pressure on outcomes in hypertensive patients. Journal of hypertension. 2012;30(4):802-10; discussion 810.
39. PAST BP Fletcher K, Mant J, McManus R, Campbell S, Betts J, Taylor C, Virdee S, Jowett S, Martin U, Greenfield S, Ford G, Freemantle N, Hobbs FD. Protocol for Past BP: a randomised controlled trial of different blood pressure targets for people with a history of stroke of transient ischaemic attack (TIA) in primary care. BMC cardiovascular disorders. 2010;10:37.
40. REIN-2 (Ramipril Efficacy in Nephropathy 2) Ruggenenti P, Perna A, Loriga G, Ganeva M, Ene-Iordache B, Turturro M, Lesti M, Perticucci E, Chakarski IN, Leonardis D, Garini G, Sessa A, Basile C, Alpa M, Scanziani R, Sorba G, Zoccali C, Remuzzi G, REIN-2 Study Group. Blood-pressure control for renoprotection in patients with non-diabetic chronic renal disease (REIN-2): multicentre, randomised controlled trial. Lancet. 2005;365(9463):939-46.
41. SPRINT (Systolic Blood Pressure Intervention Trial) SPRINT Research Group, Wright JT, Williamson JD, Whelton PK, Snyder JK, Sink KM, Rocco MV, Reboussin DM, Rahman M, Oparil S, Lewis CE, Kimmel PL, Johnson KC, Goff DC, Fine LJ, Cutler JA, Cushman WC, Cheung AK, Ambrosius WT. A Randomized Trial of Intensive versus Standard Blood-Pressure Control. The New England journal of medicine. 2015;373(22):2103-16.
42. SPS3 (Secondary Prevention of Small Subcortical Strokes Trial) McClure LA, Szychowski JM, Benavente O, Hart RG, Coffey CS. A post hoc evaluation of a sample size re-estimation in the Secondary Prevention of Small Subcortical Strokes study. Clinical trials (London, England). 2016;13(5):537-44.
43. Schrier et al (Standard versus rigorous blood pressure control) Schrier R, McFann K, Johnson A, Chapman A, Edelstein C, Brosnahan G, Ecder T, Tison L. Cardiac and renal effects of standard versus rigorous blood pressure control in autosomal-dominant polycystic kidney disease: results of a seven-year prospective randomized study. Journal of the American Society of Nephrology: JASN. 2002;13(7):1733-9.
44. Syst-Eur (Systolic Hypertension in Europe) Staessen JA, Fagard R, Thijs L, Celis H, Arabidze GG, Birkenhäger WH, Bulpitt CJ, de Leeuw PW, Dollery CT, Fletcher AE, Forette F, Leonetti G, Nachev C, O’Brien ET, Rosenfeld J, Rodicio JL, Tuomilehto J, Zanchetti A. Randomised double-blind comparison of placebo and active treatment for older patients with isolated systolic hypertension. The Systolic Hypertension in Europe (Syst-Eur) Trial Investigators. Lancet. 1997;350(9080):757-64.
45. Toto RD, Mitchell HC, Smith RD, Lee HC, McIntire D, Pettinger WA. «Strict» blood pressure control and progression of renal disease in hypertensive nephrosclerosis. Kidney international. 1995;48(3):851-9
46. UKPDS (United Kingdom Prospective Diabetes Study) Holman RR, Cull CA, Turner RC. A randomized double-blind trial of acarbose in type 2 diabetes shows improved glycemic control over 3 years (U.K. Prospective Diabetes Study 44). Diabetes care. 1999;22(6):960-4.
47. VALISH (Valsartan in Elderly Isolated Systolic Hypertension) Ogihara T, Saruta T, Rakugi H, Matsuoka H, Shimamoto K, Shimada K, Imai Y, Kikuchi K, Ito S, Eto T, Kimura G, Imaizumi T, Takishita S, Ueshima H, Valsartan in Elderly Isolated Systolic Hypertension Study Group. Target blood pressure for treatment of isolated systolic hypertension in the elderly: valsartan in elderly isolated systolic hypertension study. Hypertension. 2010;56(2):196-202.
48. Wei et al (Intensive antihypertensive treatment). Wei Y, Jin Z, Shen G, Zhao X, Yang W, Zhong Y, Wang J. Effects of intensive antihypertensive treatment on Chinese hypertensive patients older than 70 years. Journal of clinical hypertension (Greenwich, Conn.). 2013;15(6):420-7.
49. Schrier RW, Abebe KZ, Perrone RD, Torres VE, Braun WE, Steinman TI, Winklhofer FT, Brosnahan G, Czarnecki PG, Hogan MC, Miskulin DC, Rahbari-Oskoui FF, Grantham JJ, Harris PC, Flessner MF, Bae KT, Moore CG, Chapman AB, HALT-PKD Trial Investigators. Blood pressure in early autosomal dominant polycystic kidney disease. The New England journal of medicine. 2014;371(24):2255-66
50. Peng J, Lu F, Wang Z, Zhong M, Sun L, Hu N, Liu Z, Zhang W. Excessive lowering of blood pressure is not beneficial for progression of brain white matter hyperintensive and cognitive impairment in elderly hypertensive patients: 4-year follow-up study. Journal of the American Medical Directors Association. 2014;15(12):904-10.
51. Sacktor N, Gray S, Kawas C, Herbst J, Costa P, Fleg J. Systolic blood pressure within an intermediate range may reduce memory loss in an elderly hypertensive cohort. Journal of geriatric psychiatry and neurology. 1999;12(1):1-6.
52. Liu H, Gao S, Hall KS, Unverzagt FW, Lane KA, Callahan CM, Hendrie HC. Optimal blood pressure for cognitive function: findings from an elderly African-American cohort study. Journal of the American Geriatrics Society. 2013;61(6):875-81.
53. White CL, Szychowski JM, Pergola PE, Field TS, Talbert R, Lau H, Peri K, Benavente OR, Secondary Prevention of Small Subcortical Strokes Study Investigators. Can blood pressure be lowered safely in older adults with lacunar stroke? The Secondary Prevention of Small Subcortical Strokes study experience. Journal of the American Geriatrics Society. 2015;63(4):722-9.
Búsqueda y Síntesis de Evidencia
Búsqueda y síntesis de evidencia de efectos deseables e indeseables
| Grande | Moderado | Pequeño | Trivial | Varía | No lo sé |
|---|
No lo se: identificaron estudios que comparen el límite inferior de presión arterial en los rangos solicitados, relacionado a los efectos adversos.
Referencia
2. Arguedas JA, Perez MI, Wright JM. Treatment blood pressure targets for hypertension. Cochrane Database of Systematic Reviews. 2009;(3):CD004349.
3. Bangalore S., Toklu B., Gianos E., Schwartzbard A., Weintraub H., Ogedegbe G., Messerli F.H.. Optimal Systolic Blood Pressure Target After SPRINT: Insights from a Network Meta-Analysis of Randomized Trials. American Journal of Medicine. 2017;130(6):707-719.e8.
4. Bangalore S, Kumar S, Lobach I, Messerli FH. Blood pressure targets in subjects with type 2 diabetes mellitus/impaired fasting glucose: observations from traditional and bayesian random-effects meta-analyses of randomized trials. Circulation. 2011;123(24):2799-810, 9 p following 810.
5. Bavishi C, Bangalore S, Messerli FH. Outcomes of Intensive Blood Pressure Lowering in Older Hypertensive Patients. Journal of the American College of Cardiology. 2017;69(5):486-493.
6. Brunström M, Carlberg B. Effect of antihypertensive treatment at different blood pressure levels in patients with diabetes mellitus: systematic review and meta-analyses. BMJ (Clinical research ed.). 2016;352:i717.
7. Czernichow S, Zanchetti A, Turnbull F, Barzi F, Ninomiya T, Kengne AP, Lambers Heerspink HJ, Perkovic V, Huxley R, Arima H, Patel A, Chalmers J, Woodward M, MacMahon S, Neal B, Blood Pressure Lowering Treatment Trialists’ Collaboration. The effects of blood pressure reduction and of different blood pressure-lowering regimens on major cardiovascular events according to baseline blood pressure: meta-analysis of randomized trials. Journal of hypertension. 2011;29(1):4-16.
8. Ettehad D, Emdin CA, Kiran A, Anderson SG, Callender T, Emberson J, Chalmers J, Rodgers A, Rahimi K. Blood pressure lowering for prevention of cardiovascular disease and death: a systematic review and meta-analysis. Lancet (London, England). 2016;387(10022):957-67.
9. Garrison SR, Kolber MR, Korownyk CS, McCracken RK, Heran BS, Allan GM. Blood pressure targets for hypertension in older adults. Cochrane Database of Systematic Reviews. 2017;8:CD011575.
10. Kaiser T, Florack C, Stephan U, Sawicki PT. Should BP targets be lower in diabetic patients with microalbuminuria or nephropathy? A systematic review of randomised controlled trials. British Journal of Diabetes & Vascular Disease. 2003;3(4):278-281.
11. Lee M, Saver JL, Hong KS, Hao Q, Ovbiagele B. Does achieving an intensive versus usual blood pressure level prevent stroke?. Annals of neurology. 2012;71(1):133-40.
12. Lv J, Ehteshami P, Sarnak MJ, Tighiouart H, Jun M, Ninomiya T, Foote C, Rodgers A, Zhang H, Wang H, Strippoli GF, Perkovic V. Effects of intensive blood pressure lowering on the progression of chronic kidney disease: a systematic review and meta-analysis. CMAJ : Canadian Medical Association journal = journal de l’Association medicale canadienne. 2013;185(11):949-57.
13. Lv J, Neal B, Ehteshami P, Ninomiya T, Woodward M, Rodgers A, Wang H, Macmahon S, Turnbull F, Hillis G, Chalmers J, Perkovic V. Effects of intensive blood pressure lowering on cardiovascular and renal outcomes: a systematic review and meta-analysis. PLoS medicine. 2012;9(8):e1001293.
14. Malhotra R, Nguyen HA, Benavente O, Mete M, Howard BV, Mant J, Odden MC, Peralta CA, Cheung AK, Nadkarni GN, Coleman RL, Holman RR, Zanchetti A, Peters R, Beckett N, Staessen JA, Ix JH. Association Between More Intensive vs Less Intensive Blood Pressure Lowering and Risk of Mortality in Chronic Kidney Disease Stages 3 to 5: A Systematic Review and Meta-analysis. JAMA internal medicine. 2017;177(10):1498-1505.
15. McBrien K, Rabi DM, Campbell N, Barnieh L, Clement F, Hemmelgarn BR, Tonelli M, Leiter LA, Klarenbach SW, Manns BJ. Intensive and Standard Blood Pressure Targets in Patients With Type 2 Diabetes Mellitus: Systematic Review and Meta-analysis. Archives of internal medicine. 2012;172(17):1296-303.
16. Moraes AAI, Baena CP, Muka T, Bano A, Buitrago-Lopez A, Zazula A, Erbano BO, Schio NA, Guedes MH, Bramer WM, Franco OH, Faria-Neto JR. Achieved systolic blood pressure in older people: a systematic review and meta-analysis. BMC geriatrics. 2017;17(1):279.
17. Saiz, Luis Carlos, Gorricho, Javier, Garjón, Javier, Celaya, Mª Concepción, Erviti, Juan, Leache, Leire. Blood pressure targets for the treatment of people with hypertension and cardiovascular disease. Cochrane Database of Systematic Reviews. 2018;7:CD010315.
18. Turnbull F, Blood Pressure Lowering Treatment Trialists’ Collaboration. Effects of different blood-pressure-lowering regimens on major cardiovascular events: results of prospectively-designed overviews of randomised trials. Lancet. 2003;362(9395):1527-35.
19. Upadhyay A, Earley A, Haynes SM, Uhlig K. Systematic review: blood pressure target in chronic kidney disease and proteinuria as an effect modifier. Annals of internal medicine. 2011;154(8):541-8.
20. Weiss J, Freeman M, Low A, Fu R, Kerfoot A, Paynter R, Motu’apuaka M, Kondo K, Kansagara D. Benefits and Harms of Intensive Blood Pressure Treatment in Adults Aged 60 Years or Older: A Systematic Review and Meta-analysis. Annals of internal medicine. 2017;166(6):419-429.
21. Weiss J, Kerfoot A, Freeman M, Motu’apuaka M, Fu R, Low A, Paynter R, Kondo K, Kansagara D. Benefits and Harms of Treating Blood Pressure in Older Adults: A Systematic Review and Meta-analysis. VA Evidence-based Synthesis Program Reports. 2016;
22. Xie X, Atkins E, Lv J, Bennett A, Neal B, Ninomiya T, Woodward M, MacMahon S, Turnbull F, Hillis GS, Chalmers J, Mant J, Salam A, Rahimi K, Perkovic V, Rodgers A. Effects of intensive blood pressure lowering on cardiovascular and renal outcomes: updated systematic review and meta-analysis. Lancet (London, England). 2016;387(10017):435-43.
23. Tsai WC, Wu HY, Peng YS, Yang JY, Chen HY, Chiu YL, Hsu SP, Ko MJ, Pai MF, Tu YK, Hung KY, Chien KL. Association of Intensive Blood Pressure Control and Kidney Disease Progression in Nondiabetic Patients With Chronic Kidney Disease: A Systematic Review and Meta-analysis. JAMA internal medicine. 2017;177(6):792-799
24. AASK (African American Study of Kidney Disease and Hypertension). Wright JT, Bakris G, Greene T, Agodoa LY, Appel LJ, Charleston J, Cheek D, Douglas-Baltimore JG, Gassman J, Glassock R, Hebert L, Jamerson K, Lewis J, Phillips RA, Toto RD, Middleton JP, Rostand SG. Effect of blood pressure lowering and antihypertensive drug class on progression of hypertensive kidney disease: results from the AASK trial. JAMA: the journal of the American Medical Association. 2002;288(19):2421-31.
25. ABCD-2V (Appropriate Blood Pressure Control in Diabetes Part 2 with Valsartan). Estacio RO, Coll JR, Tran ZV, Schrier RW. Effect of intensive blood pressure control with valsartan on urinary albumin excretion in normotensive patients with type 2 diabetes. American journal of hypertension. 2006;19(12):1241-8.
26. ABCD-H (Appropriate blood pressure control in diabetes (hypertensive)). Estacio RO, Jeffers BW, Gifford N, Schrier RW. Effect of blood pressure control on diabetic microvascular complications in patients with hypertension and type 2 diabetes. Diabetes care. 2000;23 Suppl 2:B54-64.
27. ABCD-N (Appropriate blood pressure control in diabetes (normotensive)). Schrier RW, Estacio RO, Esler A, Mehler P. Effects of aggressive blood pressure control in normotensive type 2 diabetic patients on albuminuria, retinopathy and strokes. Kidney international. 2002;61(3):1086-97.
28. ACCORD (Action to Control Cardiovascular Risk in Diabetes). Cushman WC, Evans GW, Byington RP, Goff DC, Grimm RH, Cutler JA, Simons-Morton DG, Basile JN, Corson MA, Probstfield JL, Katz L, Peterson KA, Friedewald WT, Buse JB, Bigger JT, Gerstein HC, Ismail-Beigi F. Effects of intensive blood-pressure control in type 2 diabetes mellitus. The New England journal of medicine. 2010;362(17):1575-85
29. BBB (Behandla Blodtryck Bättre [Treat Blood Pressure Better in Swedish]). Hannson L. The BBB Study: the effect of intensified antihypertensive treatment on the level of blood pressure, side-effects, morbidity and mortality in «well-treated» hypertensive patients. Behandla Blodtryck Bättre. Blood pressure. 1994;3(4):248-54.
30. Cardio-Sis (Italian Study on the Cardiovascular Effects of Systolic Blood Pressure Control). Verdecchia P, Staessen JA, Angeli F, de Simone G, Achilli A, Ganau A, Mureddu G, Pede S, Maggioni AP, Lucci D, Reboldi G, Cardio-Sis investigators. Usual versus tight control of systolic blood pressure in non-diabetic patients with hypertension (Cardio-Sis): an open-label randomised trial. Lancet. 2009;374(9689):525-33.
31. ESCAPE (Effect of Strict Blood Pressure Control and ACE Inhibition on the Progression of CRF in Pediatric Patients) ESCAPE Trial Group, Wühl E, Trivelli A, Picca S, Litwin M, Peco-Antic A, Zurowska A, Testa S, Jankauskiene A, Emre S, Caldas-Afonso A, Anarat A, Niaudet P, Mir S, Bakkaloglu A, Enke B, Montini G, Wingen AM, Sallay P, Jeck N, Berg U, Caliskan S, Wygoda S, Hohbach-Hohenfellner K, Dusek J, Urasinski T, Arbeiter K, Neuhaus T, Gellermann J, Drozdz D, Fischbach M, Möller K, Wigger M, Peruzzi L, Mehls O, Schaefer F. Strict blood-pressure control and progression of renal failure in children. The New England journal of medicine. 2009;361(17):1639-50.
32. HOMED-BP (Hypertension Objective treatment based on Measurement by Electrical Devices of Blood Pressure) Asayama K, Ohkubo T, Metoki H, Obara T, Inoue R, Kikuya M, Thijs L, Staessen JA, Imai Y, Hypertension Objective Treatment Based on Measurement by Electrical Devices of Blood Pressure (HOMED-BP). Cardiovascular outcomes in the first trial of antihypertensive therapy guided by self-measured home blood pressure. Hypertension research: official journal of the Japanese Society of Hypertension. 2012;35(11):1102-10.
33. HOT (Hypertension Optimal Treatment) Hansson L, Zanchetti A, Carruthers SG, Dahlöf B, Elmfeldt D, Julius S, Ménard J, Rahn KH, Wedel H, Westerling S. Effects of intensive blood-pressure lowering and low-dose aspirin in patients with hypertension: principal results of the Hypertension Optimal Treatment (HOT) randomised trial. HOT Study Group. Lancet. 1998;351(9118):1755-62.
34. INVEST (International Verapamil SR/Trandolapril Study) Pepine CJ, Handberg EM, Cooper-DeHoff RM, Marks RG, Kowey P, Messerli FH, Mancia G, Cangiano JL, Garcia-Barreto D, Keltai M, Erdine S, Bristol HA, Kolb HR, Bakris GL, Cohen JD, Parmley WW. A calcium antagonist vs a non-calcium antagonist hypertension treatment strategy for patients with coronary artery disease. The International Verapamil-Trandolapril Study (INVEST): a randomized controlled trial. JAMA: the journal of the American Medical Association. 2003;290(21):2805-16.
35. JATOS 2008 (JATOS 2008) JATOS Study Group. Principal results of the Japanese trial to assess optimal systolic blood pressure in elderly hypertensive patients (JATOS). Hypertension research: official journal of the Japanese Society of Hypertension. 2008;31(12):2115-27.
36. Lewis JB, Berl T, Bain RP, Rohde RD, Lewis EJ. Effect of intensive blood pressure control on the course of type 1 diabetic nephropathy. Collaborative Study Group. American journal of kidney diseases : the official journal of the National Kidney Foundation. 1999;34(5):809-17.
37. MDRD (Modification of Diet in Renal Disease) Sarnak MJ, Greene T, Wang X, Beck G, Kusek JW, Collins AJ, Levey AS. The effect of a lower target blood pressure on the progression of kidney disease: long-term follow-up of the modification of diet in renal disease study. Annals of internal medicine. 2005;142(5):342-51
38. Okin PM, Hille DA, Kjeldsen SE, Dahlöf B, Devereux RB. Impact of lower achieved blood pressure on outcomes in hypertensive patients. Journal of hypertension. 2012;30(4):802-10; discussion 810.
39. PAST BP Fletcher K, Mant J, McManus R, Campbell S, Betts J, Taylor C, Virdee S, Jowett S, Martin U, Greenfield S, Ford G, Freemantle N, Hobbs FD. Protocol for Past BP: a randomised controlled trial of different blood pressure targets for people with a history of stroke of transient ischaemic attack (TIA) in primary care. BMC cardiovascular disorders. 2010;10:37.
40. REIN-2 (Ramipril Efficacy in Nephropathy 2) Ruggenenti P, Perna A, Loriga G, Ganeva M, Ene-Iordache B, Turturro M, Lesti M, Perticucci E, Chakarski IN, Leonardis D, Garini G, Sessa A, Basile C, Alpa M, Scanziani R, Sorba G, Zoccali C, Remuzzi G, REIN-2 Study Group. Blood-pressure control for renoprotection in patients with non-diabetic chronic renal disease (REIN-2): multicentre, randomised controlled trial. Lancet. 2005;365(9463):939-46.
41. SPRINT (Systolic Blood Pressure Intervention Trial) SPRINT Research Group, Wright JT, Williamson JD, Whelton PK, Snyder JK, Sink KM, Rocco MV, Reboussin DM, Rahman M, Oparil S, Lewis CE, Kimmel PL, Johnson KC, Goff DC, Fine LJ, Cutler JA, Cushman WC, Cheung AK, Ambrosius WT. A Randomized Trial of Intensive versus Standard Blood-Pressure Control. The New England journal of medicine. 2015;373(22):2103-16.
42. SPS3 (Secondary Prevention of Small Subcortical Strokes Trial) McClure LA, Szychowski JM, Benavente O, Hart RG, Coffey CS. A post hoc evaluation of a sample size re-estimation in the Secondary Prevention of Small Subcortical Strokes study. Clinical trials (London, England). 2016;13(5):537-44.
43. Schrier et al (Standard versus rigorous blood pressure control) Schrier R, McFann K, Johnson A, Chapman A, Edelstein C, Brosnahan G, Ecder T, Tison L. Cardiac and renal effects of standard versus rigorous blood pressure control in autosomal-dominant polycystic kidney disease: results of a seven-year prospective randomized study. Journal of the American Society of Nephrology : JASN. 2002;13(7):1733-9.
44. Syst-Eur (Systolic Hypertension in Europe) Staessen JA, Fagard R, Thijs L, Celis H, Arabidze GG, Birkenhäger WH, Bulpitt CJ, de Leeuw PW, Dollery CT, Fletcher AE, Forette F, Leonetti G, Nachev C, O’Brien ET, Rosenfeld J, Rodicio JL, Tuomilehto J, Zanchetti A. Randomised double-blind comparison of placebo and active treatment for older patients with isolated systolic hypertension. The Systolic Hypertension in Europe (Syst-Eur) Trial Investigators. Lancet. 1997;350(9080):757-64.
45. Toto RD, Mitchell HC, Smith RD, Lee HC, McIntire D, Pettinger WA. «Strict» blood pressure control and progression of renal disease in hypertensive nephrosclerosis. Kidney international. 1995;48(3):851-9
46. UKPDS (United Kingdom Prospective Diabetes Study) Holman RR, Cull CA, Turner RC. A randomized double-blind trial of acarbose in type 2 diabetes shows improved glycemic control over 3 years (U.K. Prospective Diabetes Study 44). Diabetes care. 1999;22(6):960-4.
47. VALISH (Valsartan in Elderly Isolated Systolic Hypertension) Ogihara T, Saruta T, Rakugi H, Matsuoka H, Shimamoto K, Shimada K, Imai Y, Kikuchi K, Ito S, Eto T, Kimura G, Imaizumi T, Takishita S, Ueshima H, Valsartan in Elderly Isolated Systolic Hypertension Study Group. Target blood pressure for treatment of isolated systolic hypertension in the elderly: valsartan in elderly isolated systolic hypertension study. Hypertension. 2010;56(2):196-202.
48. Wei et al (Intensive antihypertensive treatment). Wei Y, Jin Z, Shen G, Zhao X, Yang W, Zhong Y, Wang J. Effects of intensive antihypertensive treatment on Chinese hypertensive patients older than 70 years. Journal of clinical hypertension (Greenwich, Conn.). 2013;15(6):420-7.
49. Schrier RW, Abebe KZ, Perrone RD, Torres VE, Braun WE, Steinman TI, Winklhofer FT, Brosnahan G, Czarnecki PG, Hogan MC, Miskulin DC, Rahbari-Oskoui FF, Grantham JJ, Harris PC, Flessner MF, Bae KT, Moore CG, Chapman AB, HALT-PKD Trial Investigators. Blood pressure in early autosomal dominant polycystic kidney disease. The New England journal of medicine. 2014;371(24):2255-66
50. Peng J, Lu F, Wang Z, Zhong M, Sun L, Hu N, Liu Z, Zhang W. Excessive lowering of blood pressure is not beneficial for progression of brain white matter hyperintensive and cognitive impairment in elderly hypertensive patients: 4-year follow-up study. Journal of the American Medical Directors Association. 2014;15(12):904-10.
51. Sacktor N, Gray S, Kawas C, Herbst J, Costa P, Fleg J. Systolic blood pressure within an intermediate range may reduce memory loss in an elderly hypertensive cohort. Journal of geriatric psychiatry and neurology. 1999;12(1):1-6.
52. Liu H, Gao S, Hall KS, Unverzagt FW, Lane KA, Callahan CM, Hendrie HC. Optimal blood pressure for cognitive function: findings from an elderly African-American cohort study. Journal of the American Geriatrics Society. 2013;61(6):875-81.
53. White CL, Szychowski JM, Pergola PE, Field TS, Talbert R, Lau H, Peri K, Benavente OR, Secondary Prevention of Small Subcortical Strokes Study Investigators. Can blood pressure be lowered safely in older adults with lacunar stroke? The Secondary Prevention of Small Subcortical Strokes study experience. Journal of the American Geriatrics Society. 2015;63(4):722-9.
Búsqueda y Síntesis de Evidencia
Búsqueda y síntesis de evidencia de efectos deseables e indeseables
| Muy baja | Baja | Moderada | Alta | Ningún estudio incluído |
|---|
Ningún estudio incluído: No se encontraron estudios que respondieran la preguntan de interés, por lo tanto existe considerable incertidumbre respecto del efecto de «Límite inferior de presión arterial diastólica (PAD) en 70 mm de Hg.» en comparación a «Límite inferior de presión arterial diastólica (PAD) en 60 mm de Hg.».
Evidencia de investigación
|
Desenlaces |
Certeza de la Evidencia |
|
Beneficio |
⨁◯◯◯ |
|
Efectos adversos |
⨁◯◯◯ |
| Incertidumbre o variabilidad importantes | Posiblemente hay incertidumbre o variabilidad importantes | Probablemente no hay incertidumbre ni variabilidad importantes | No hay variabilidad o incertidumbre importante |
|---|
No hay variabilidad o incertidumbre importante: En función de la evidencia de investigación, experiencia clínica, conocimiento de gestión o experiencia de las personas con la condición o problema de salud, el equipo elaborador de la Guía consideró que no existe incertidumbre o variabilidad importante respecto a lo que escogería una persona informada de los efectos deseables e indeseables del «Límite inferior de presión arterial diastólica (PAD) en 70 mm de Hg.» y «Límite inferior de presión arterial diastólica (PAD) en 60 mm de Hg.». Todas o casi todas las personas escogerían tener el ímite inferior de presión arterial diastólica (PAD) en 70 mm de Hg.
Evidencia de investigación
No se encontraron artículos sobre valores y preferencias de pacientes que pudieran responder esta pregunta.
Búsqueda y Síntesis de Evidencia
Búsqueda y síntesis de evidencia de valores y preferencias de los pacientes
| Favorece la comparación | Probablemente favorece la comparación | No favorece la intervención ni la comparación | Probablemente favorece la intervención | Favorece la intervención | Varía | No lo sé |
|---|
Favorece la intervención: Considerando que la intervención es «Límite inferior de presión arterial diastólica (PAD) en 70 mm de Hg.» y la comparación es «Límite inferior de presión arterial diastólica (PAD) en 60 mm de Hg.», el equipo elaborador de la Guía opinó que el balance entre efectos deseables e indeseables claramente favorece al «Límite inferior de presión arterial diastólica (PAD) en 70 mm de Hg.»
| Costos extensos | Costos moderados | Costos y ahorros despreciables | Ahorros moderados | Ahorros extensos | Varía | No lo sé |
|---|
Costos y ahorros despreciables: El equipo elaborador de la Guía consideró que los costos y ahorros de «Límite inferior de presión arterial diastólica (PAD) en 70 mm de Hg.» son despreciables si se compara con «Límite inferior de presión arterial diastólica (PAD) en 60 mm de Hg.», en función de los antecedentes, experiencia clínica, conocimiento de gestión o experiencia de los pacientes.
Evidencia de investigación
A continuación se muestran los costos referenciales, es preciso considerar que estos costos fueron recogidos con el único objetivo de constituir un antecedente aproximado del tratamiento de caries no cavitada sin compromiso pulpar en dentición primaria con ionómero de alta densidad y con restauraciones con resina compuesta de modo que el equipo elaborador de la Guía se pudiese pronunciar respecto.
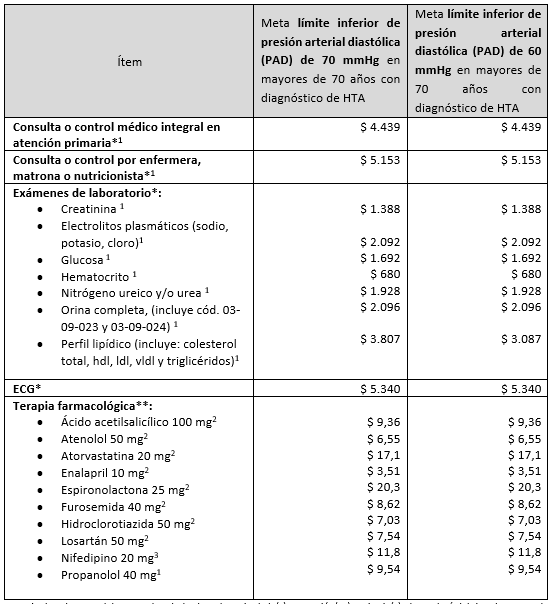
El porcentaje de cobertura del seguro de salud sobre el precio de la(s) prestación(es) sanitaria(s), dependerá del tipo de seguro de cada paciente.
* Precios referenciales por paciente considerando frecuencia cada vez.
**Precios referenciales por comprimido
Búsqueda y Síntesis de Evidencia
Búsqueda de costos
| Favorece la comparación | Probablemente favorece la comparación | No favorece la intervención ni la comparación | Probablemente favorece la intervención | Favorece la intervención | Varía | Ningún estudio incluído |
|---|
Ningún estudio incluído: No se realizó la búsqueda de estudios que abordaran la costo-efectividad, ya que la intervención evaluada no es considerada de alto costo (Anual $2.418.399 y Mensual $201.533) (1).
1. Ministerio de Salud. Decreto 80: Determinar umbral nacional de costo anual al que se refiere el artículo 6° de la Ley 20.850 [Internet]. Santiago; 2015 Nov.
| Reducido | Probablemente reducido | Probablemente ningún impacto | Probablemente aumentado | Aumentado | Varía | No lo sé |
|---|
Aumentado: El equipo elaborador de la Guía consideró que la equidad en salud aumentaría si se recomendase «Límite inferior de presión arterial diastólica (PAD) en 70 mm de Hg.», dado que en la actualidad existe acceso, ya sea en términos económicos, geográficos u otros.
| No | Probablemente no | Probablemente sí | Sí | Varía | No lo sé |
|---|
Sí: El equipo elaborador de la Guía consideró que «Límite inferior de presión arterial diastólica (PAD) en 70 mm de Hg.» SÍ es aceptable para las partes interesadas (profesionales de la salud, gestores de centros de salud, directivos de centros de salud, pacientes, cuidadores, seguros de salud, otros).
| No | Probablemente no | Probablemente sí | Sí | Varía | No lo sé |
|---|
Sí: El equipo elaborador de la Guía consideró que «Límite inferior de presión arterial diastólica (PAD) en 70 mm de Hg.» SÍ es factible implementar, contemplando la capacidad de la red asistencial, los recursos humanos disponibles a nivel país, recursos financieros, etc.
